What is the facial nerve?
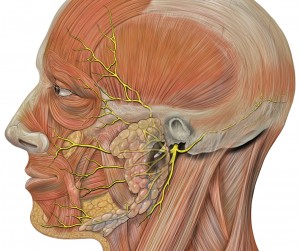
The facial nerve or 7th cranial nerve is known as a “cranial nerve” since it starts in the brain. It sends branches out to the face, neck, tongue, salivary glands (secrete saliva into the mouth), and the outer ear. A normal functioning nerve allows us to move our face (smile, frown, pout), purse our lips to whistle and move the neck to make “scary faces.” Some nerves that travel with the facial nerve, or “piggyback,” allow us to taste with the front of our tongue, make saliva in the mouth and let us feel the outside of our ear canal.
What problems can develop with the facial nerve?
Problems with the facial nerve result in weakness or paralysis of the face muscles and possibly, a loss of taste on the affected side. This nerve loss is one of the most disfiguring since it involves facial movement. Without the nerve connection (innervation) intact, the eye does not close, there is loss of facial muscle tone, and movement on the affected side is reduced or lost.
What causes paralysis of the facial nerve?
It is important to understand the location or pathway the facial nerve takes in the head and face. This understanding makes it easier to see how the nerve is damaged and how this damage may affect function.
The facial nerve starts in the brain, and then tracks through a narrow space located inside the ear (internal auditory canal). The nerve then passes through the middle ear (behind the ear drum) and leaves through another narrow passage located under the ear area (stylomastoid foramen). It then branches out to provide muscle movement and sensation to various parts of the face and neck. The branches start inside the parotid gland (in front of the ear) and travel to the forehead, cheek, nose, mouth and neck.
Anything that may cause swelling or pressure on the nerve can result abnormal function.
Some of the general causes of problems along the pathway of the facial nerve include; congenital (birth) abnormalities, infections of the middle ear (OTITIS MEDIA), or CHOLESTEATOMA, infections or tumors of the PAROTID GLAND, FACIAL AND NECK TRAUMA, and uncommonly, as a complication after an operation in the ear area (for example, after a MASTOIDECTOMY). One of the most common causes of facial nerve paralysis a viral infection called Bell’s Palsy.
How is facial paralysis evaluated?
Evaluation begins with thorough history to help determine the cause. A physical examination will help to determine whether the nerve damage is at the brain level (central) or closer to the ear and face area (peripheral).
Usually various tests are performed as part of the evaluation. The nerve (8th cranial nerve) that allows us to hear is located close to the facial nerve, so it may also be affected (sensorineural hearing loss) when the facial nerve is paralyzed. In addition, problems with the middle ear may also be associated with a hearing loss similar to having the sensation of earplugs in the ears (conductive hearing loss). The type of hearing loss, if present, helps with diagnosis and treatment of the condition.
A thorough examination is performed to determine the level of the paralysis. The extent of facial nerve paralysis can involve all of the nerve (complete) or just a part of the nerve (incomplete).
An x-ray is usually performed after the history and physical examination of the patient. A computed tomography (CT) scan or magnetic resonance imaging (MRI) scan is very useful in making the diagnosis. It can help to determine exactly where swelling, infection, trauma, or tumor may be that is causing the facial nerve abnormality.
More specialized tests involve the use of electrical impulses. A commonly used technique called electromyography (EMG) sends electrical impulses to muscle (as a nerve would do). This is a painless technique that helps to determine whether the problem is with the nerve or the muscle itself.
Another study is known as the nerve excitability test (NET). This study uses electrical impulses to compare the normal facial nerve on one side of the face with the abnormal one on the other. Electroneurobility testing (ENoG) goes further than NET, by giving actual numbers to help with the comparison.
Finally, a group of tests checking tear production, saliva production, taste sensation and small ear muscle movement can help to determine if only a small branch of the facial nerve is damaged. This is known as topographic localization.
When would an Otolaryngologist be consulted to help manage facial paralysis?
An Otolaryngologist is consulted to help surgically treat many causes of facial nerve paralysis that will not resolve on their own. These conditions include a trapped nerve that needs to be released to function normally, which can be seen with FACIAL TRAUMA, tumors, or severe OTITIS MEDIA. The otolaryngologist is also skilled in surgically connecting a facial nerve that has been divided by trauma.
In these instances, the facial nerve will continue to die until a surgical procedure is undertaken. This underscores the urgency in which facial nerve paralysis should be evaluated.